Radicular Cyst
- Odontogenic cyst of inflammatory origin
- Preceeded by pulp necrosis and chronic periapical granuloma
- Most common odontogenic cyst
- Also known as periapical cyst
- Described as a residual cyst if present following tooth extraction
- Lateral radicular cyst - occasionally form at the side of a non-vital tooth as a result of the opening of a lateral branch of the root canal
Epidemiology[edit | edit source]
- Commonest type of jaw cyst (~60% of all cases)
- Most common between ages of 20-60yrs old – rare <10yrs old
- ♂ > ♀ (3:2)
- Maxilla > Mandible (3:1)
- Incidence of different types of radicular/peripical cysts:
- Apical - 70%
- Lateral - 20%
- Residual - 10%
Clinical Features[edit | edit source]
- Slowly progressive painless swellings
- Usually cause no symptoms unless large enough to be conspicuous
- Can get infected → painful and rapid expansion (inflammatory oedema)
- If visible, swelling is usually round and hard
- If left to enlarge →
- Bone can be reduced to egg shell thickness and a crackling sensation may be felt on gentle pressure
- Finally if part of the wall is resorbed entirely the swelling is soft, fluctuant and bluish in colour
- A necrotic tooth from which the tooth has originated is (by definition) present (if not then the cyst is termed a residual cyst)
Differential Diagnosis[edit | edit source]
- Other cysts of the jaws
Aetiology and Pathogenesis[edit | edit source]
Aetiology[edit | edit source]
- Radicular cysts are cysts of inflammatory origin
- Preceded by necrotic tooth and periodical granuloma
Pathogenesis[edit | edit source]
- Major factors in the pathogenesis of cyst formation:
- Proliferation of epithelial lining and fibrous capsule
- Apical periodontitis → resorption of alveolar bone via immune-inflammatory process
- Inflammtory cytokines and growth factors released in apical periodontitis can stimulate epithelial cell rests of Malassez (remnants of Hertwig's epithelial root sheath)
- Basal cells of the epithelial cell rests of Malassez are stimulated to proliferate and form the cyst
- Hydrostatic pressure of cyst fluid
- Cyst fluid (inflammortary exudate and necrotic cellular debris) contains straw-coloured fluid containing cholesterol cystals with protein content >5g/dL
- ∴ osmostic tension can cause cysts to expand in balloon like fashion
- Expansion tends to occur in pathway of least resistance therefore tend to be less destructive
- Hydrostatic pressure within cysts is ~70cm of water (higher than the capillary blood pressure)
- Resorption of surrounding bone
- Cyst tissues have been shown to release bone-resorbing factors (prostaglandin E2 and E3) and collagenases
- It is not fully clear what affect these have on cyst growth
- Proliferation of epithelial lining and fibrous capsule
Investigations[edit | edit source]


Imaging[edit | edit source]
Plain film[edit | edit source]
- Commonly an incidental finding on routine intra-oral or panoramic radiographs
- Cysts only make up ~15% of all periapical radiolucencies[2]
- Consider a cyst as opposed to periapical abscess when lesion is larger than 2cm2[3]
- Common radiographic features:
- Round radiolucent area
- Unilocular
- Sharply defined
- Condensed radio-opaque periphery is present in long standing cysts
- Associated with necrotic tooth
- Large lesions can cause displacement/tilting of adjacent teeth
- Large cysts in maxilla may extend in irregular shapes
- Infected cyst may cause hazy outline and resorption of surrounding bone
Computed Tomography[edit | edit source]
- Can facilitate diagnosis, and 3D characterisation for surgical planning
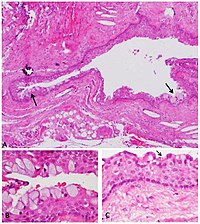
Histopathology[edit | edit source]
- Common histopathological findings:
- Epithelial lining
- Stratified squamous epithelium (non-keratinised) - except when near maxillary sinus where there is respiratory epithelium (pseudostratified ciliated columnar epithelium)
- Varying thickness
- Lacks well defined basal cell layer (may be missing)
- Hyaline bodies and mucous cells may be present ∵ of metaplasia
- Longstanding cysts = thin epithelial lining, thick fibrous wall and minimal inflammatory infiltrate
- Cyst capsule and wall
- Collagenous fibrous connective tissue
- Vascular during active growth
- Clefts
- Clefts are present in cyst capsule
- These occur ∵ breakdown of blood cells → cholesterol formation → cholesterol then dissolves out → clefts
- Cyst fluid
- Usually watery and opalescent
- Sometimes viscid and yellowish
- Microscopy (after smear) shows cholesterol crystals
- Histology shows protein (broken down leucocytes and cells distended within fat globules)
- Epithelial lining
Management[edit | edit source]
- Cyst enucleation - usually treatment of choice along with one of the following:
- Orthograde endodontic treatment
- Apicectomy
- Extraction
- Orthograde endodontic treatment alone is suitable for small cysts (<1cm) as the cyst may subsequently heal
- Marsupialization may sometimes be needed for very large cysts
Prognosis and Complications[edit | edit source]
- Recurrence is uncommon if capsule is completely removed
Follow-up[edit | edit source]
- Routine follow-up not needed
- Suitable for results to be given to patient via remote consultation/mail
References[edit | edit source]
- ↑ AboulHosn M, Noujeim Z, Nader N, Berberi A. Decompression and enucleation of a mandibular radicular cyst, followed by bone regeneration and implant-supported dental restoration. Case reports in dentistry. 2019 Jan 9;2019.
- ↑ Nair PN. New perspectives on radicular cysts: do they heal?. International endodontic journal. 1998 May 1;31(3):155-60.
- ↑ Natkin E, Oswald RJ, Carnes LI. The relationship of lesion size to diagnosis, incidence, and treatment of periapical cysts and granulomas. Oral Surgery, Oral Medicine, Oral Pathology. 1984 Jan 1;57(1):82-94.