Basal Cell Carcinoma
Jump to navigation
Jump to search
Commonest form of skin cancer
Slow growing tumour affecting the basal cells of the skin
Can locally invade but rarely metastasises
Can sometimes be referred to by laymen as "rodent ulcer"
Epidemiology[edit | edit source]
- Accounts for 80% of non-melanoma skin cancers
- 80% of cases occur in the head and neck [1]
- Marked geographical variation (commonest in Europe, Australia and USA)
- Much more common in fair-skinned individuals with a family history
- Up to 30% of caucasians will develop BCCs in their lifetime [1]
- Incidence increases in those >50 years old
- Multiple BCCs in younger patients is suggestive of nevoid basal-cell carcinoma syndrome (Gorlin-Goltz Syndrome)
- ♀ > ♂
Clinical Features[edit | edit source]
- Most commonly affects sun exposed areas
- Most BCCs remain localised
- Growth rate is variable but patients tend to report slow growing lesion
- Patients often give a history of a "spot" that occasionally bleeds
- Different clinical subtypes exist which tend to occur at different anatomical locations (see below for main types)
- Nodular and superficial BCCs can produce pigment → pigmented BCCs (~7% of cases)[2]
Differential Diagnosis[edit | edit source]
- Squamous Cell Carcinoma
- Malignant melanoma (pigmented basal cell carcinoma)
- Melanocytic naevi (pigmented basal cell carcinoma)
- Bowen's disease (especially superficial basal cell carcinoma)
- Psoriasis (superficial)
- Eczema (superficial)
- Sebaceous hyperplasia
- Molluscum contagiosum
- Appendygeal tumours
Aetiology and Pathogenesis[edit | edit source]
Aetiology[edit | edit source]
- The exact cause of BCC is unknown
- Risk factors
- Ultraviolet (UV) light exposure from sun/sun-beds, especially in childhood [3]
- Genetic predisposition/association with fair skin type (Fitzpatrick I + II)
- Immunosuppression (post-transplant, anti-TNF drugs [infliximab], haematological malignancies)
- Arsenic exposure
- Previous BCC - 50% will develop second BCC within 5 years
- Nevoid basal-cell carcinoma syndrome (Gorlin-Goltz Syndrome)
- Xeroderma pigmentosum
- Bazex-Dupré-Christol syndrome
Pathogenesis[edit | edit source]
- Majority of cases exhibit UV radiation-induced carcinogenesis
- 90% of cases demonstrate alterations genes causing a hyper activation of the hedgehog (HH) protein family [4]
- This is a pathway involved in organogenesis and tissue repair
- Includes PTCH1 receptor, SMO signal transducer and GLI transcription factors
- TP53 mutations are the second most important gene mutation - 20-60% [4]
Investigations[edit | edit source]
Diagnosis is usually clinical
Dermatoscope may assist in clinic diagnosis
In cases where there is uncertainty an incisional or punch biopsy may be performed
Dermatoscopy[edit | edit source]


Histopathology[edit | edit source]
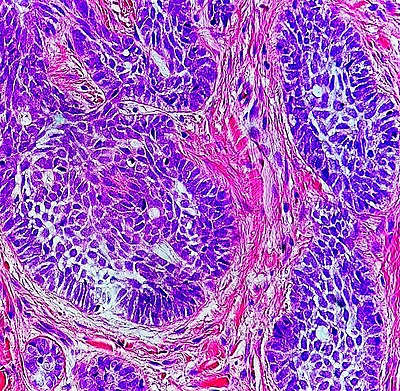
- Common histological features of BCC are:
- Nodules and/or strands of atypical basaloid cells that show nuclear palisading, cellular apoptosis, and scattered mitotic activity in the dermis
- Artifactual cleft formation may be seen between the tumour lobules and the surrounding stroma
- Solar elastosis is usually present in the dermis
- Histological subtypes:
| Type | Description | Aggressive |
|---|---|---|
| Nodular | Discrete nests of basaloid cells in the dermis. There is peripheral palisading of the malignant keratinocytes and a mucinous-surrounding tumour stroma. Between the tumor and the dermis, a separation or "cleft," is often apparent due to retraction artifact in tissue processing | No |
| Superficial | Foci of malignant, basaloid, palisading tumours "budding" off the epidermis | No |
| Pigmented | Presence of melanin and melanophages within the tumour nodules | No |
| Morphoeic/Infiltrative | Thin cords of basaloid tumor cells penetrating the surrounding collagen, which may appear sclerotic | Yes |
| Micronodular | Numerous small collections of malignant basaloid cells within the dermis and exhibit more subtle findings of peripheral palisading and retraction compared with nodular BCCs | Yes |
| Basosquamous | These have a component of nodular or superficial BCC overlying an invasive portion that has features of BCC and SCC | Yes |
- Perivascular or perineural invasion are features associated with the most aggressive tumours
Imaging[edit | edit source]
CT or MRI imaging may be used for extensive lesions to delineate any involvement in adjacent structures (especially if there are concerns that the tumour may have invaded major nerves, the orbit or the parotid gland)
Management[edit | edit source]
Risk Stratification[edit | edit source]

- Clinical criteria for high risk lesions:
- Location: Mask areas of the face (see diagram)
- Size: >10mm (note that for most of trunk an extremities the criteria is >20mm)
- Recurrent tumour
- Patient on immunosuppression
- Tumour in site of previous radiotherapy
- Pathological criteria for high risk lesions:
- Infiltrative growth pattern (infiltrating, morphoeic, micronodular)
- Basosquamous
- Level of invasion is beyond subcutaneous fat
- >6mm tumour thickness
- Perineural invasion (named nerve or nerve with diameter >0.1mm)
- pT2 >20mm / pT3 / pT4
- Bone invasion
- Involved margins (0mm) or histologically close margins (<1mm)
Patient Counselling[edit | edit source]
- Discuss different treatment options, especially in context of scars and the implication of that for the patient
- Sun protection advice (and the implication of this on vitamin D levels)
- Discuss the increased risk of developing new primary skin cancers (∴ they need to remain vigilant for early detection and treatment)
Multidisciplinary Team[edit | edit source]
- There are 2 levels of MDT for skin cancers:
- Local skin multidisciplinary team (LSMDT) → usually found in district general hospitals
- Specialised skin multidisciplinary team (SSMDT) → usually located in teaching hospitals with cancer centres
- Cases requiring discussion at LSMDT:
- Incompletely excised BCCs (consider referral to SSMDT where Mohs is to be offered
- Cases requiring discussion at SSMDT:
- Complex Mohs cases (complex reconstruction / rare tumours)
- Large / locally advanced BCC or BCCs requiring complex reconstruction
- Metastatic BCC
Surgical Treatment[edit | edit source]
- Standard surgical excision with pre-determined margins
- Suitable for the majority of BCCs (should be offered as first line treatment for all low-risk and high-risk with well defined margins)
- A 3mm clinical margin achieves clearance in 85% of cases whilst a 4-5mm margin achieves clearance in 95% of cases
- In primary morphoeic BCC: 3mm margin → 66% clearance; 5mm → 82%; 13mm → 95%
- Recommendations for surgical margins:
- Low risk lesions → 4mm peripheral margin
- High risk lesion → 5mm peripheral margin
- Deep margin should be to a clear plane (including cuff of fat if present or other deep structures if needed)
- Morphoeic BCC → 13mm peripheral margins
- Mohs micrographic surgery
- Microscopically controlled surgery that aims to confirm removal of all tumour histologically prior to reconstruction
- Labour intensive
- Consider in:
- Recurrent tumours
- High risk tumours
- Where minimal tissue loss is essential (e.g. anatomically sensitive areas such as peri-orbital)
- Slow Mohs = Excise → wait for H&E result → delayed reconstruction
- Destructive surgical techniques
- Not recommended for high risk lesions
- Curettage and cautery
- Cryosurgery: liquid nitrogen
- Laser therapy: CO2 or pulse dye lasers can be used
Non-surgical Treatment[edit | edit source]
- Topical therapy
- Imiquimod →
- Immune modulator. 5x/week for 6 weeks. Can cause local reactions (skin discomfort) and flu-like symptoms. 84% cure rates.
- 5-Fluorouracil cream →
- Chemotherapeutic aged. OD or BD for 3-4 weeks. Causes local reactions as above but no flu-like symptoms. ?higher rates of wound infection
- Imiquimod →
- Photodynamic therapy
- Suitable for low risk superficial BCCs
- Uses light and a photosensitising chemical substance (methyl aminolevulinate [MAL] or aminolevulinic acid [ALA])
- Comparable cure rates to topical therapy
- Electrochemotherapy
- Not currently recommended for BCCs
- Radiotherapy
- Treatment of choice if patient refuses or is unable to tolerate surgery and treatment of the lesion is needed
- Usually utilised superficial electrons
- Can be single fraction (higher complications) or fractionated (usually 5 doses - less complications and higher cure rate)
- Complications of radiotherapy:
- Soft tissue radionecrosis
- Cataracts
- Telangiectasia
- Secondary RT-induced cancers
- Higher recurrence rates that with surgery (10%)
Prognosis and Complications[edit | edit source]
- Incomplete excision
- Discuss at LSMDT
- Radial margin:
- Low risk lesions → Offer re-excision / Mohs / Observation / Other treatment options
- High risk lesions → Offer re-excision / Mohs / Radiotherapy
- Deep margin → Offer re-excision / Mohs / Radiotherapy
- Recurrence
- 5-year recurrence rate is[6]:
- ~5% for all cases following surgical excision with predetermined margins
- 0.5% for cases with clear margins
- 0.3-6.5% following Mohs in the head and neck
- Treating already recurrent tumours is associated with higher subsequent recurrent rates, ranging from 4% to 10%
- 10% for lesions treated with radiotherapy alone
- 5-year recurrence rate is[6]:
- Advanced/metastatic BCC
- Metastatic BCC is rare
- No standard therapy for this group; clinical trials appropriate if available
- Use of oral/topical hedgehog pathway inhibitors (e.g. vismodegib) has been shown to be effective in patients with advanced, multiple, or metastatic BCC - funding limited in UK
Follow-up[edit | edit source]
- Completely excised BCCs / BCCs treated by Mohs do not routinely need follow up
- Patients with possibly involved / close radial margins, complex repairs, post radiotherapy, or with multiple tumours may require follow up tailored to the individuals clinical picture
References[edit | edit source]
- ↑ 1.0 1.1 Wong CS, Strange RC, Lear JT. Basal cell carcinoma. Bmj. 2003 Oct 2;327(7418):794-8.
- ↑ Maloney ME, Jones DB, Sexton FM. Pigmented basal cell carcinoma: investigation of 70 cases. Journal of the American Academy of Dermatology. 1992 Jul 1;27(1):74-8.
- ↑ Corona R, Dogliotti E, D'Errico M, Sera F, Iavarone I, Baliva G, Chinni LM, Gobello T, Mazzanti C, Puddu P, Pasquini P. Risk factors for basal cell carcinoma in a Mediterranean population: role of recreational sun exposure early in life. Archives of dermatology. 2001 Sep 1;137(9):1162-8.
- ↑ 4.0 4.1 Pellegrini C, Maturo MG, Di Nardo L, Ciciarelli V, Gutiérrez García-Rodrigo C, Fargnoli MC. Understanding the molecular genetics of basal cell carcinoma. International journal of molecular sciences. 2017 Nov;18(11):2485.
- ↑ 5.0 5.1 Lallas A, Apalla Z, Argenziano G, Longo C, Moscarella E, Specchio F, Raucci M, Zalaudek I. The dermatoscopic universe of basal cell carcinoma. Dermatology practical & conceptual. 2014 Jul;4(3):11.
- ↑ 6.0 6.1 Nasr I, McGrath EJ, Harwood CA, Botting J, Buckley P, Budny PG, Fairbrother P, Fife K, Gupta G, Hashme M, Hoey S. British Association of Dermatologists guidelines for the management of adults with basal cell carcinoma 2021. British Journal of Dermatology. 2021 May 29.


